 We deliver a suite of revenue cycle management and health information management services to leading hospitals, health systems, physician groups, software companies, medical facilities and healthcare providers across the country. Our commitment seeks to exceed world class standards in quality, accuracy, turnaround time and security, resulting in extraordinary outcomes for our clients.
We deliver a suite of revenue cycle management and health information management services to leading hospitals, health systems, physician groups, software companies, medical facilities and healthcare providers across the country. Our commitment seeks to exceed world class standards in quality, accuracy, turnaround time and security, resulting in extraordinary outcomes for our clients.
Banerasoft is a Medical Coding and Billing services company that offer’s customized service at an affordable price. We make the difference for you; we only get paid when you get paid.
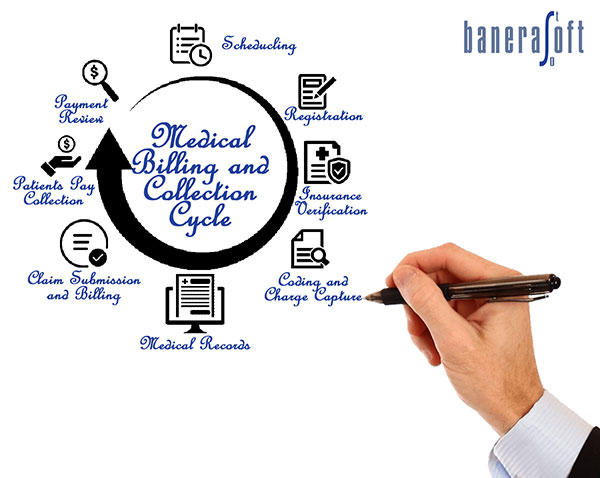
Banerasoft provides a full suite of end-to-end revenue cycle management services for hospitals, professional billing and ambulatory surgery centres. Utilizing our deep knowledge of best practices in revenue cycle management, we deliver high-quality and cost-effective solutions for our clients. Our highly specialized teams work to streamline operations, decrease insurance claim denials and maximize revenue while maintaining compliance within industry regulations. With turnaround times between 24-48 hours, our clients are assured of accurate, timely, and balanced results.
Offering customized revenue cycle solutions tailored to each client:
Our medical billing services are focused on your bottom-line. We customize medical billing, medical coding and accounts receivables as per your needs, so that you can focus on your core area.
As a Medical Billing Services company, we have the experience and expertise you need to increase your revenues and decrease your expenses. We have helped many clients to save up to 50% on their overall expenses. Our experienced staff with our state-of-the- art infrastructure helps to accelerate your cash flow. Our certified billers and coders provide high quality coding, billing and revenue cycle management.
 Provide us the software platform and clearing house and we do the rest, making Banerasoft your go-to partner for any revenue cycle management needs.
Provide us the software platform and clearing house and we do the rest, making Banerasoft your go-to partner for any revenue cycle management needs.
 Our specialized coding expertise optimizes our client accuracy rates, turnaround times, productivity and need for flexibility.
Our specialized coding expertise optimizes our client accuracy rates, turnaround times, productivity and need for flexibility.
We follow these processes to accomplish quality-driven results for our clients:
 Technology is the backbone of our solutions.
Technology is the backbone of our solutions.
Our experienced software team has deep domain expertise as well as technical skills on trending platforms.
A dedicated team to help improve productivity and quality, having consistently delivered >99% accuracy through our services.
Our IT services and consulting speed time to market, lower ownership costs and increase ownership values for our payer clients. We deploy data mining, statistics, modelling, machine learning, and artificial intelligence to make predictions about likely business outcomes that help clients sustain their competitive advantage.
IT professionals who work on cutting-edge technologies, data scientists, and analytical thinkers who live inside the data. We align closely with the business needs, goals, culture, and core values of our clients.
 Banerasoft specializes in process improvement to enhance revenue and streamline operations.
Banerasoft specializes in process improvement to enhance revenue and streamline operations.
Maximizing accuracy at every point in the claims payment process is essential if payers are to compete. By utilizing our payer assistance services, Banerasoft is able to enhance accuracy and drive revenue for our clients.
Our analytics solutions identify the foundational objectives important to your organization, then deliver business and clinical value by providing actionable insights from your data that lead to intelligent and knowledge-based decisions.
The focus of Revenue Cycle Analytics is to streamline and improve the revenue cycle process by capturing the maximum amount of revenue at the ideal level of cost containment.
Banerasoft specializes in healthcare revenue cycle analytics aimed at providing a complete snapshot of business functionality. These include: